A Manual of Laboratory and Diagnostic Tests serves as a comprehensive guide, providing essential details on various procedures, from blood work to imaging studies, ensuring accurate patient care.
1.1 Overview of Common Laboratory Tests
Common laboratory tests include blood tests, such as CBC and differential, to assess blood disorders. Urinalysis detects kidney and urinary tract issues, while imaging studies like X-rays and CT scans reveal internal injuries or abnormalities. These tests provide crucial data for diagnosis and treatment planning, effectively guiding clinical decisions and ensuring accurate patient care.
1.2 Importance of Diagnostic Testing in Healthcare
Diagnostic testing is integral to modern healthcare, enabling early detection, accurate diagnosis, and effective treatment planning. It helps identify abnormalities, monitor chronic conditions, and prevent complications. By providing critical data, these tests guide clinical decision-making, ensuring personalized patient care. Diagnostic testing also enhances patient outcomes by confirming the presence or absence of diseases, enabling timely interventions. This process is vital for improving healthcare efficiency and reducing costs, making it a cornerstone of evidence-based medicine.
Categories of Laboratory Tests
Laboratory tests are categorized into blood, urine, and imaging studies, each assessing specific bodily functions to detect abnormalities, diagnose conditions, and guide treatment plans effectively.
2.1 Blood Tests: Complete Blood Count (CBC) and Differential
A Complete Blood Count (CBC) and differential are essential blood tests that measure various components of blood, including red and white blood cell counts, hemoglobin, and platelets.
These tests help diagnose conditions like anemia, infections, and blood disorders by providing insights into the body’s overall health and immune response.
A differential further breaks down white blood cells to identify specific types, aiding in pinpointing infections or inflammatory processes.
Regular monitoring of these tests is crucial for early detection of abnormalities and guiding appropriate treatment plans.
2.2 Urinalysis and Urine Culture
Urinalysis is a routine test that examines urine for abnormal substances like protein, glucose, and blood, helping diagnose conditions such as kidney disease or diabetes.
A urine culture identifies pathogens causing infections, guiding antibiotic treatment.
These tests are crucial for detecting urinary tract infections (UTIs) and monitoring chronic conditions.
Proper sample collection is essential to ensure accurate results, making urinalysis and culture vital tools in early detection and targeted therapy for urinary disorders;
2.3 Imaging Studies: X-rays, CT Scans, and MRIs
Imaging studies like X-rays, CT scans, and MRIs are non-invasive tools that provide detailed images of internal structures.
X-rays are commonly used to diagnose fractures or lung conditions.
CT scans offer cross-sectional views, ideal for detecting injuries or abnormalities in organs.
MRIs use magnetic fields to produce high-resolution images of soft tissues, such as the brain or joints.
These modalities help healthcare providers visualize and diagnose a wide range of conditions, from bone fractures to internal organ diseases.

Preparation and Collection of Samples
Proper preparation and collection of samples are crucial for accurate test results. Following protocols ensures reliable outcomes. Using correct equipment and techniques maintains sample integrity. Safety measures prevent contamination and exposure, ensuring both patient and handler protection.
3.1 Patient Preparation for Blood Draws
Proper patient preparation for blood draws ensures accurate test results and minimizes complications. Fasting may be required for certain tests, while hydration is essential for others. Patients should rest for 10–15 minutes before the draw to stabilize vital signs. Avoiding contaminants like food or medications is crucial. Clear communication about the procedure helps reduce anxiety. Verifying patient identity and test orders before proceeding is vital for safety and accuracy. Adherence to these steps ensures reliable outcomes and a smooth process for both patients and healthcare providers.
3.2 Proper Technique for Collecting Urine Samples
Collecting urine samples requires attention to detail to ensure accuracy and avoid contamination. Patients should use a sterile container provided by healthcare professionals. Midstream collection is often recommended to minimize contamination from skin flora. Proper hand hygiene and cleaning of the genital area are essential. First-morning samples are typically most concentrated and preferred for certain tests. Labels should be applied immediately, and samples should be stored appropriately until analysis. Adherence to these steps ensures reliable results and maintains patient safety.
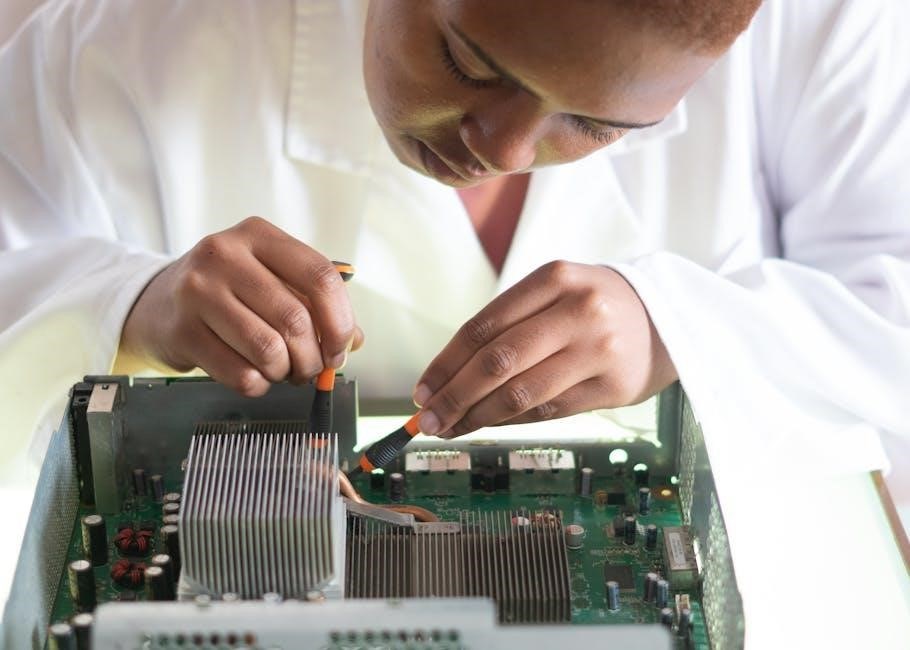
3.3 Safety Precautions for Handling Biological Specimens
Handling biological specimens requires strict adherence to safety protocols to prevent exposure and contamination. Always wear Personal Protective Equipment (PPE), including gloves, lab coats, and eye protection. Ensure specimens are stored in leak-proof, labeled containers. Use biosafety cabinets for high-risk samples. Avoid direct contact with potentially infectious materials. Properly disinfect surfaces and equipment after use. Dispose of biohazardous waste in designated containers. Follow laboratory guidelines and receive regular training to maintain a safe working environment and protect both patients and healthcare workers.

Interpretation of Test Results
Interpreting test results is crucial for accurate diagnosis and treatment. Understanding normal and abnormal values, correlating findings with symptoms, and ensuring result accuracy are key. Clinicians rely on these insights to guide patient care effectively.
4.1 Understanding Normal and Abnormal Values
Understanding normal and abnormal values is critical for interpreting laboratory results. Reference ranges are established based on population data, and deviations may indicate health issues. Factors like age, gender, and medical conditions can influence results. Abnormal values trigger further investigation, while normal values rule out certain conditions. Accurate interpretation requires context, including clinical symptoms and patient history, to ensure proper diagnosis and treatment. This step is vital for making informed healthcare decisions.
4.2 Correlating Test Results with Clinical Symptoms
Correlating test results with clinical symptoms is essential for accurate diagnosis. Laboratory values must be interpreted in the context of the patient’s presentation, medical history, and physical findings. For example, elevated white blood cell counts may indicate infection or inflammation. Clinicians must consider factors like age, comorbidities, and medications that could influence results. Discrepancies between test results and symptoms warrant further investigation. This integrated approach ensures timely and effective patient care, guiding treatment decisions and improving outcomes.

Diagnostic Imaging Techniques
Diagnostic imaging techniques, such as X-rays, CT scans, and MRIs, are crucial for visualizing internal structures. They help detect fractures, soft tissue injuries, and internal abnormalities, guiding precise diagnoses and treatments.
5.1 Ultrasound and Its Clinical Applications
Ultrasound imaging is a non-invasive diagnostic tool using high-frequency sound waves to produce real-time images of internal structures. It is widely used in obstetrics, cardiology, and abdominal imaging. Key applications include fetal monitoring during pregnancy, assessing blood flow in vessels, and detecting conditions like gallstones or liver disease. Ultrasound is painless, radiation-free, and highly effective for guiding biopsies or drainage procedures, making it a versatile and essential modality in modern healthcare settings.
5.2 Mammography and Other Radiographic Exams
Mammography is a specialized radiographic exam used to detect breast abnormalities, including cancer, through low-dose X-rays. It is a key tool in early detection, improving treatment outcomes. Other radiographic exams include X-rays, CT scans, and MRIs, each providing detailed images of internal structures. These tests are essential for diagnosing fractures, lung diseases, and soft tissue injuries. Regular mammography screenings are recommended for women over 40 to ensure early detection and timely intervention, making it a cornerstone in preventive care.

Specialized Tests and Studies
Specialized tests include advanced diagnostics like tumor markers, oncology testing, and cardiac stress tests. These studies provide detailed insights into specific conditions, aiding in precise diagnosis and treatment planning.
6.1 Cardiac Stress Tests and Echocardiograms
Cardiac stress tests assess heart function under physical exertion, detecting potential ischemia or arrhythmias. Echocardiograms use ultrasound to visualize heart structures, evaluating valve function and cardiac chamber sizes. These tests are crucial for diagnosing coronary artery disease, cardiomyopathies, and valvular abnormalities. They guide treatment decisions, such as angioplasty or medication therapy, ensuring personalized care for patients with cardiovascular conditions. Both tests are non-invasive and provide critical insights into cardiac health, aiding in early intervention and improved patient outcomes.
6.2 Tumor Markers and Oncology Testing
Tumor markers are substances in blood, tissue, or urine that may indicate cancer. Common markers include PSA for prostate cancer and CA-125 for ovarian cancer. Oncology testing involves analyzing these biomarkers to diagnose, monitor, and manage cancer. Such tests help assess treatment response and detect recurrence early. Advanced techniques like molecular diagnostics further refine cancer detection, enabling targeted therapies. These tools are vital for personalized oncology care, improving patient outcomes and streamlining treatment plans.

Emerging Trends in Diagnostic Testing
Emerging trends in diagnostic testing include point-of-care testing, advancements in molecular diagnostics, and the rise of personalized medicine, enhancing accuracy and patient care.
7.1 Point-of-Care Testing (POCT) and Its Advantages
Point-of-Care Testing (POCT) enables rapid diagnostic testing near or at the patient’s site, improving timely decision-making and patient outcomes. Its advantages include convenience, speed, and cost-effectiveness, allowing healthcare providers to make immediate clinical decisions. POCT reduces the need for lab visits, enhances patient monitoring, and empowers healthcare professionals with real-time data. Common examples include glucose meters and rapid COVID-19 tests. This approach is particularly beneficial in remote or resource-limited settings, ensuring equitable access to diagnostics and improving overall healthcare delivery.
7.2 Advances in Molecular Diagnostics
Advances in molecular diagnostics have revolutionized healthcare by enabling precise identification of genetic, infectious, and oncologic conditions. Techniques like PCR (Polymerase Chain Reaction) and Next-Generation Sequencing (NGS) allow for rapid and accurate detection of pathogens and genetic mutations. These tools enhance personalized medicine, enabling tailored treatments and early intervention. Molecular testing also supports monitoring of treatment response and disease progression, improving patient outcomes. Its integration into clinical practice has transformed how diseases are diagnosed and managed, offering hope for earlier and more effective interventions.
Clinical Considerations
Clinical considerations involve ensuring patient confidentiality, adhering to ethical standards, and applying evidence-based practices. Proper handling of biological specimens and accurate test interpretations are critical for reliable outcomes.
8.1 Testing in Special Populations: Pediatrics and Geriatrics
Testing in pediatric and geriatric populations requires special considerations due to age-related physiological differences. For children, smaller sample sizes and age-specific reference ranges are crucial. In geriatrics, chronic conditions and polypharmacy often necessitate tailored approaches. Ethical considerations, such as informed consent and patient autonomy, must be prioritized. These populations benefit from personalized care to ensure accurate diagnoses and appropriate interventions, addressing their unique healthcare needs effectively.
8.2 Ethical and Legal Aspects of Diagnostic Testing
Ethical and legal considerations in diagnostic testing ensure patient safety, privacy, and informed consent. Adhering to regulations like HIPAA protects patient data. Clinicians must interpret results responsibly, avoiding misuse. Legal compliance and ethical practices build trust in healthcare delivery, ensuring transparency and accountability. These principles guide healthcare professionals in providing accurate and respectful care, balancing patient rights with medical responsibilities effectively.
Diagnostic testing is vital for accurate patient care. Future advancements, like point-of-care and molecular diagnostics, will enhance efficiency. This manual remains a key guide for healthcare education and practice.
9.1 The Role of Nurses in Diagnostic Testing
Nurses play a critical role in diagnostic testing by preparing patients, collecting specimens, and ensuring accurate results. They serve as liaisons between lab technicians and healthcare providers, facilitating timely interventions. Nurses also educate patients about test procedures and results, fostering trust and adherence to treatment plans. Their attention to detail and patient-centered care enhance the reliability of diagnostic outcomes, making them indispensable in modern healthcare settings.
9.2 Continuous Education and Updates in Diagnostic Practices
Continuous education is vital for healthcare professionals to stay updated on advancements in diagnostic practices. With the rapid evolution of technology and testing methods, ongoing learning ensures accurate and effective patient care. Resources like A Manual of Laboratory and Diagnostic Tests and platforms like Medbridge provide essential updates, enabling professionals to adapt to new guidelines and improve diagnostic accuracy. Regular training enhances proficiency, ensuring optimal patient outcomes and adherence to best practices in healthcare settings.
